Comment; It is a problem, yet an understandable one. Few physicians are truly Lyme-literate, the infection is hard to diagnose with contradictory criteria from major organizations, false-negative labs common etc. Additionally numerous treatment modalities generally mean there is no 100% effective “gold standard” treatment-failures of treatment occur, followed by difficulty in diagnosis once again…
MenuHEALTHWhat Happens When Lyme Disease Becomes an Identity?
Maybe It’s Lyme
What happens when illness becomes an identity?
By Molly FischerIllustration: Art Handler, Photo by Flashpop/Getty/Getty Images

Polly Murray, in the 1960s and ’70s, was a mother of four with an old house on several acres in Lyme, Connecticut. In the summer, her kids built forts in the woods; they ice-skated on frozen cow ponds in the winter. The Murrays had an idyllic life in the country. They also had enormous rashes, strange joint swellings, and recurrent fevers.
One son wound up in the infirmary at boarding school, unable to lift his leg. Another had to have the fluid drained from his knee. Murray was constantly taking herself or her husband or one of her kids to a doctor — but none of the doctors ever had answers, nor did they seem especially interested in finding any. So Murray took the search upon herself. In The Widening Circle, her 1996 memoir, she reproduces extracts from her diary (“Monday, July 28: Todd had a fever of 100 again for two days and a severe jaw ache; he said it hurt to open his mouth … The attack lasted for five days”). The record Murray gathered is a testament to both the relentlessness of the symptoms and her own relentlessness in tracking them. Her husband compares her to “the lonely hero of a Hitchcock movie”: isolated, embattled, and disbelieved.
Soon, though, Murray started to hear other stories like hers. Her area, it appeared, had a cluster of juvenile-rheumatoid-arthritis cases. She called the state’s health department and met with Dr. Allen Steere, a rheumatologist doing a fellowship at Yale. He pored over her pages of notes. On the car ride home, Murray wept with joy: Steere didn’t have any answers, but he had listened. He wanted to find out what was wrong. By 1976, the condition Murray had observed had become known as Lyme disease.
“Lyme disease was a disease born of advocacy,” Dr. Paul Auwaerter told me. Auwaerter, whose lab focuses on Lyme and other tick-borne diseases, is the clinical director of the Division of Infectious Diseases at Johns Hopkins University School of Medicine. Back in the ’70s, Murray and her fellow Connecticut mothers had to fight for attention. Their experience left behind a powerful legacy, Auwaerter said, a sense that perhaps “the medical establishment didn’t really listen initially or were trying to be dismissive.”
Decades after Polly Murray kept her diary of symptoms, the spirit of advocacy associated with Lyme disease endures. But while Murray’s efforts were ultimately vindicated by medical science, a new fight — for the recognition of something known as “chronic Lyme,” which can encompass a vast range of symptoms and need not be linked to any tick bite — has grown into a phenomenon often untethered from scientific method or peer review. The chronic-Lyme community has a new agenda, one that was visible at last fall’s Global Lyme Alliance Gala in New York, where supporters gathered at Cipriani heard a speech from Real Housewife of Beverly Hills Yolanda Hadid.Get unlimited access to The Cut and everything else New York.LEARN MORE »
On the show, Hadid’s diagnosis had became a major plotline; it represented a breakthrough moment in pop-culture Lyme-disease awareness. Two of her children, the models Bella and Anwar Hadid, also have Lyme diagnoses. They join an assortment of famous and fame-adjacent spokespeople who have “opened up” about Lyme: Avril Lavigne, Kelly Osbourne, Ally Hilfiger, Crystal Hefner, and Rob Thomas’s wife, Marisol. Hadid’s speech at the gala was brief — she was in the midst of a relapse, she said, so she hadn’t really been able to write anything — but the hardest part about having Lyme disease, she told the crowd, was people not believing she had Lyme disease. “My biggest struggle every day was people telling me that maybe I have Munchausen disease,” Hadid said. “ ‘How can she look so beautiful and be so sick?’ ‘How can she be in bed seven days a week and then show up to work?’ Well, I did,” she said. And then, to applause, “Because I’m a badass Dutch girl. But it wasn’t easy.”
This is the rallying cry of the Lyme Warrior. Spend a while browsing #lymewarrior on Instagram and what you find looks like wellness content at first. There are selfies, shots of food, talk of toxins, exhortations toward self-care. There are more extensive arrays of supplements than you might expect. Then the IVs snake into view. There are hospital gowns and seats at outpatient-treatment centers and surgically implanted ports displayed with pride. This is wellness predicated on the constant certainty that all is not well. Like Hadid, the Lyme Warriors struggle against those who would doubt their condition, and, like Hadid, they are firm in their resolve. They have a name, and they have each other.
Where Murray sought to answer a question, the warrior who now takes up the cause of chronic Lyme is seeking to affirm an answer. For this community of patients, Lyme has come to function as something more expansive than a diagnosis. While Lyme disease is a specific medical condition — one that may manifest more severely or less, be treated more easily or less — chronic Lyme is something else altogether. (The medical establishment generally avoids using the term chronic Lyme, and because of this establishment wariness, advocates who believe Lyme is a chronic infection now sometimes advise patients to avoid it too.) This version of Lyme has no consistent symptoms, no fixed criteria, and no accurate test. This Lyme is a kind of identity. Lyme is a label for a state of being, a word that conveys your understanding of your lived experience. Lyme provides the language to articulate that experience and join with others who share it. In the world of chronic Lyme, doctors are trustworthy (or not) based on their willingness to treat Lyme. Tests are trustworthy (or not) based on their ability to confirm Lyme. Lyme is the fundamental fact, and you work backward from there. Lyme is a community with a cause: the recognition of its sufferers’ suffering — and, with it, the recognition of Lyme.
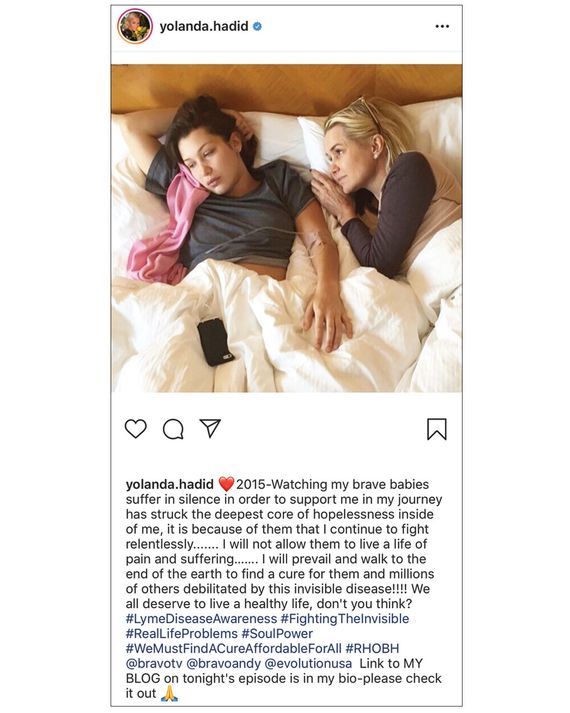
Bella and Yolanda Hadid on Instagram.Photo: Instagram
The home page of Lyme Resource Medical of New York shows Central Park, with distant sunbathers scattered across a rolling expanse of grass. While the name suggests a degree of institutional grandeur, Lyme Resource Medical is primarily the practice of Dr. Bernard Raxlen, and its offices are a small fifth-floor warren of rooms near Times Square.
Raxlen is one of the first names you’ll find if you search for a Lyme-disease doctor in New York. The Lyme community’s word-of-mouth network makes certain doctors — like Richard Horowitz, the best-selling author of Why Can’t I Get Better — into niche celebrities, and within this milieu, Raxlen has the status of an elder statesman. Twenty years ago, he was one of the doctors who founded ILADS, the International Lyme and Associated Diseases Society, which issues its own treatment guidelines, intended to counter those of the medical establishment. He inspires fierce reverence among patients. “Tears streamed down my face,” wrote Jennifer Crystal of watching him speak at a 2012 ILADS conference. Crystal, whom Raxlen began treating in 2005, blogs about chronic Lyme for the Global Lyme Alliance. (Her recent posts include one on an experience she calls “song iteration” — having songs stuck in her head for “days, weeks, even a month” — which she describes as a “maddening symptom of neurological Lyme disease.”) Allie Cashel, another longtime patient of Raxlen’s, is the author of Suffering the Silence: Chronic Lyme Disease in an Age of Denial, a 2015 memoir that begins when she comes into Raxlen’s care as a child after he diagnoses her Wall Street father with chronic Lyme. “Thank God for Dr. Raxlen,” Cashel’s father tells her. “He had the guts to go against a lot of conventional wisdom, and I will be forever grateful to him for that.”
You are unlikely to find yourself in this office unless you’re already considering the possibility that you have Lyme disease — perhaps you saw something online or heard something from a friend. Still, a Lyme-literate doctor like Raxlen is the gatekeeper who validates chronic Lyme as an identity. Lyme-literate doctors are often referred to as LLMDs, though the title doesn’t reflect any specific set of qualifications or credentials. ILADS offers a daylong course in Lyme fundamentals and, through its educational arm, the International Lyme and Associated Diseases Educational Foundation (ILADEF), a one-to-two-week training program for clinicians. The only prerequisites for the latter are completion of the Lyme-fundamentals course and the ability to prescribe antibiotics.
When I visited, Raxlen’s waiting room had two black leather couches and a narrow bookcase in one corner. Among the titles on its shelves were The Creator and the Cosmos: How the Greatest Scientific Discoveries of the Century Reveal God and Get Rich Click! The Ultimate Guide to Making Money on the Internet. As I waited for him to finish an appointment, I read a children’s book I’d found among the issues of WebMD magazine on the coffee table. Learning About Lyme is written by Raxlen and relates the story of a little girl named Annie. “Annie has been real sad lately,” reads one page. “Her personality has changed from bright and sunny to dark and moody. Drastic changes in your personality can be a sign of Lyme disease.”
From Raxlen’s office in the back drifted snatches of conversation. “I could get bit again?” said a woman’s voice. “Oh yeah, I’m not going on the lawn at all!” A few minutes later, a woman in gym clothes with long blonde hair and a tight face emerged. She took a seat on the other couch and began to fill out a sheaf of paperwork.
Raxlen brought me back to his office, past a wall with a large black-and-white photo of himself in younger days, when his rakish goatee was still dark. The CV posted on the Lyme Resource Medical site lists stints in Guatemala, Hawaii, Israel, and Brazil; not until he’d settled in Connecticut and was practicing as a family therapist did he turn his focus to Lyme disease. He is trained as a psychiatrist, but he is not board certified in that or any other specialty.
When a new patient arrives in Raxlen’s office, “you test them first,” he told me. “You’d send the blood to a — ” He paused and seemed to consider the next word. “A respectable lab. The bigger labs don’t usually get it right.
Their tests are pretty antiquated.” The mainstream testing process for Lyme measures a patient’s antibodies, which has made it a source of consternation: Within the first week or so after infection, a patient may not yet have an immune response sufficient to show up on the test and could produce a false negative. (“From that has sprung the sense, often advocated, that the test is not very good at understanding the symptoms,” Johns Hopkins’s Auwaerter said. “When, in fact, I think it is very good.”) Lyme-literate doctors will ask that patients do their testing through specialty Lyme labs that apply their own criteria in measuring results and describe their offerings as “more sensitive.” Among the most prominent is IGeneX, a Bay Area lab whose founder and longtime CEO was a co-founder of ILADS.
Even so, having done the test, “you don’t believe the test,” Raxlen told me. “Too many people are sent away with a diagnosis of NLD — not Lyme disease. And that’s because the tests come back negative. You can’t rely on the test to differentiate a Lyme case. You must go by the clinical symptoms.” Diagnosis is a matter of trusting “your own radar,” he said.
The simplest, standard-issue textbook case of Lyme looks like this: A tick carrying the disease bites a person, who then develops an expanding bull’s-eye rash around the bite. (This happens in some 70 to 80 percent of cases, according to the CDC.) This is the point at which the person would probably see a doctor, who’d prescribe a short course of antibiotics. A sufferer might also miss the rash and seek treatment later, after developing Lyme’s other early symptoms, like a fever or painful swollen joints. A doctor in a Lyme-endemic area (like the East Coast or the Upper Midwest) would then administer a two-tier test for Lyme antibodies and prescribe antibiotics if it came back positive. But there can be complications or extreme cases, which include infection of the brain and nervous system. Sometimes people don’t notice a bite or don’t develop a rash, so they never get diagnosed and the disease progresses and grows severe. And some patients who have been treated for Lyme experience lingering symptoms afterward — sometimes referred to as post-treatment Lyme disease, or PTLD.
No one disputes that Lyme disease can leave patients with long-term symptoms; the source of disagreement is their cause. Is the illness the aftereffect of an infection that has passed? Or is it an ongoing, active infection, the kind that might require continued treatment with antibiotics? At present, the vast majority of mainstream medical authorities do not support the use of long-term antibiotics for persistent Lyme symptoms; this includes the Centers for Disease Control, the National Institutes of Health, the American Academy of Neurology, the American College of Rheumatology, and the Infectious Diseases Society of America.
Yet there are just enough openings in the standard account of Lyme disease — enough ambiguities about how this disease looks, how it works, and how it can be stopped — to make it sound like a conceivable explanation for all kinds of symptoms. Start looking online and the symptoms that chronic-Lyme patients describe may well sound familiar. “Brain fog” is the big one everyone talks about: trouble thinking and focusing, forgetfulness. Then there’s fatigue and pain — headaches, joint pain, muscle pain that won’t go away. Or maybe the pain does go away — it comes and goes. Or maybe there’s nausea. Or your eyes hurt. Or you’ve got panic attacks or bladder issues. For years, syphilis was known as “the great imitator,” but lately advocates of chronic Lyme have claimed this title for their own condition. Lyme, they explain, could look like anything. It might be the cause behind any number of other diseases, recognized (Alzheimer’s, multiple sclerosis) or otherwise. One booklet I picked up at a Lyme support group included a list of recommended films and books, the last of which was Morgellons: The Legitimization of a Disease: A Factual Guide by the World’s Leading Clinical Expert. “Morgellons” is the diagnosis adopted by a community of patients who believe that medically unidentifiable parasites under their skin are causing sores that extrude fibers, fuzz, and thread. Morgellons, according to the booklet, is “a mysterious emerging infection of the skin that seems to be correlated with Lyme disease.” (The ILADS archive of research by members also includes work on Morgellons.)
Lyme is an infectious disease, which sets it apart from other diagnoses that patients with ongoing exhaustion and pain might receive, such as chronic-fatigue syndrome or fibromyalgia. The explanation for suffering that Lyme offers is almost folkloric in its appeal. The tick, an unseen vampire parasite, emerges from the wilderness — from any green place — to bite. Like Snow White’s apple or Sleeping Beauty’s spindle, it leaves behind a not-quite-deadly curse. The fact of a bite (remembered or otherwise) gives the diagnosis its visceral power. It resonates with the earliest, storybook understanding of disease: You’ve got a bug, the germs made you sick, so you must kill them with the right medicine to get well. An autoimmune disorder is confusing; a bite is clarifying. A bite means this illness came from outside. This is an invasion, a kind of possession. This is not part of you.
The bacterium itself is often anthropomorphized in the chronic-Lyme world: It’s devious, sneaky, hiding out in your organs, claiming control of your body. Illness can manifest years after a possible tick bite, can disappear and return later. Lyme becomes the organizing principle through which a patient understands his or her body, which makes it hard to say whether it is ever really gone. Every migraine, every fever, every unexplained ache could be further evidence of Lyme. Its explanatory power is absolute.
Today, chronic-Lyme advocates speak of being erased, victimized, silenced, and marginalized; they blame the medical establishment’s rejection of their claims on ignorance and bias. In 2017, at the Global Lyme Alliance’s first event outside the Northeast, GLA CEO Scott Santarella said, according to one blogger in attendance, “There is no other disease in the world where the patients are treated so unjustly.”
Last year, the writer Porochista Khakpour published a memoir about chronic Lyme that cast the condition in these terms. Her book, called Sick,received favorable reviews in The New Yorker and elsewhere. Recently, Khakpour tweeted that she believed she’d been passed over for jobs in the past year because of discrimination against her chronic illness. “A lot of you are getting sick & joining our masses,” she added. “Everything ‘wrong’ with me is also what is powerful about me. You ableds are [crying] about hangnails; we disableds are [cradling] our own hearts through every beat.” Lena Dunham, who got the word SICK tattooed across the back of her neck in April, wrote a post that same month for the Instagram community Sick Sad Girlz Club. “I have never been well,” Dunham wrote. “I don’t know what people mean when they say ‘I’m fine’ … I try and create awareness wherever I can for the issues I live with — OCD, endometriosis, Ehlers-Danlos syndrome, fibromyalgia, chronic Lyme. But I also worry it’s too much of a mouthful, that nobody will believe so many diagnoses because ya can’t get struck by lightning twice. It’s all interconnected, I explain. I’m the scientist, the historian, the comedian — just trying to figure out how.”
Because of chronic Lyme’s status outside the medical establishment, patient statistics are hard to come by, but a 2009 study in the Journal of Women’s Health reviewed trials of antibiotic treatment for chronic Lyme in which 69 percent of patients were women. This preponderance of female patients has lately brought the debate over chronic Lyme into the context of a much larger issue: medicine’s historic, systemic tendency to dismiss and devalue women’s agency and their knowledge of their own bodies. Women with conditions like endometriosis have long experienced doctors waving off their complaints; who could blame them (or anyone who’s heard their stories) for some baseline mistrust of mainstream medicine? Dr. Rachel Pearson, a pediatrician, is the author of No Apparent Distress, a memoir dealing with injustice in the American health-care system, and last summer, she wrote an essay for the New York Review of Books about her experiences with chronic-Lyme patients. Pearson told me she thinks of herself as a feminist clinician; she doesn’t want to “do this thing of undercutting women’s stories or parents’ stories.” When she writes, though, she wants to think through clinical situations that challenge her in fundamental ways. Encounters between mainstream doctors and chronic-Lyme patients are a prime example, one she compares to the experience of treating anti-vaxxers: “Chronic Lyme becomes an identity, being anti-vax becomes an identity, and once a belief is incorporated into someone’s identity, it’s very hard to counter.”
Robert A. Aronowitz is chair of the Department of History and Sociology of Science at the University of Pennsylvania; he studies the history of disease and the shifting ways people understand what illness means. Murray’s diagnosis, he pointed out, arrived not long before patient activism emerged as a force in the treatment of AIDS and breast cancer. Yet in contrast to ongoing advocacy around those conditions, the work of patient activists on behalf of Lyme focuses on what the disease even is, who has it in the first place, and who decides.
This is the essential question for Lyme, said Aronowitz. “It’s the matter of who gets to define the disease at all.”

Lena Dunham on Instagram. Photo: Instagram
Once Bernard Raxlen, the midtown doctor, has diagnosed a patient with Lyme, he places him or her on a regimen of herbs and supplements — “supplements that treat biofilm. Supplements that treat cystic forms, and so on,” he said. These include turmeric and oregano, as well as liquid stevia drops. “Then you have the oral antibiotics, and you don’t just stay with doxycycline” — that is, the standard mainstream treatment for Lyme disease. “There are many which are used, and you rotate them so as not to build resistance.” If treatment with oral antibiotics fails to produce results, “after a certain designated period of time, somewhere between three to six months, you would change your course of direction into an intravenous protocol.” He estimates that between 20 and 30 percent of his patients require this treatment, which he recommends they undergo for “no less than six months.”
Long-term antibiotics are a treatment whose benefits have not been demonstrated in controlled scientific studies. Unlike many unproven treatments, however, they have real, well-established risks — risk for individual patients but also the risk of contributing to antibiotic-resistant bacteria globally. The World Health Organization calls antibiotic resistance “one of the biggest threats to global health, food security, and development today.”
Some of these drugs’ risks are routine: Long-term antibiotics, for example, often mean long-term diarrhea. PICC lines and Hickman catheters — implanted ports used to administer IV drugs — always create the potential for infection. Patients under treatment for chronic Lyme have died of infected catheters and C. difficile diarrhea. The common intravenous antibiotic ceftriaxone, or Rocephin, can cause serious gallbladder problems like cholecystitis, according to studies — in the ’90s, a cluster of cases in a New Jersey hospital were linked to treatment for “unsubstantiated diagnoses” of Lyme disease.
And here is the crux of the medical establishment’s objection to the treatment of chronic Lyme, the source of the mutual distrust between the chronic-Lyme community and mainstream medicine: the demand for a treatment as extreme as long-term and intravenous antibiotics. From a mainstream medical perspective, Aronowitz explained, the situation is something akin to patients who have not been diagnosed with cancer deciding to seek out “cancer-literate” doctors willing to administer chemotherapy. “It wouldn’t be just like, ‘Oh, there’s an alternative construction of things, let people be people.’ ” After all, “ ‘Do no harm’ is the first ethical principle in medicine.”
Patients come to a doctor like Raxlen despite a multitude of things you might think would keep them away. Not least among these is the expense: A first visit, which lasts two hours, costs $1,350 out of pocket; subsequent visits, every couple of months, are $600.
Before people arrive in a Lyme-literate doctor’s office, they’ve often pursued mainstream care, too. Patient narratives often include the testimony of seeing five, ten, or 15 other doctors before receiving a Lyme diagnosis. Lyme patients, in other words, tend to be people who can afford to go to the doctor, be dismissed, and find another doctor. Raxlen himself put it more bluntly: “It’s a rich man’s illness.” Alternatively, it is an illness to empty the bank account of anyone but a rich man. (Steve Cohen, the hedge-fund billionaire purported to have inspired Billions, has committed more than $60 million to Lyme and tick-borne-disease causes. His wife, Alexandra, is a chronic-Lyme patient. Several universities that pursue research topics friendly to the chronic-Lyme cause — such as Columbia and Tulane — are among the recipients of his largesse.)Lyme was certainty. Lyme was authority and answers.
Near the end of my conversation with Raxlen, I mentioned how clear it is that people crave answers — that they want some label to help them understand the things they’re going through. Raxlen agreed. Was it ever hard for him not to provide that, I wondered, if he wasn’t certain that what they were experiencing was Lyme?
“I’m pretty sure when I tell the patient what I think is going on and why and document it for them,” he said, “and show them what tests were negative and why it can’t be A or B, but now we’re confronted with what’s inside this C boundary and everything’s fitting in, then I can tell the patient, from my experience, I’m pretty sure this is what’s going on.”
And, I asked, sometimes the answer isn’t Lyme?
He cut me off. “The lady that was sitting there that was marking off the forms has a 19- or 20-year history of living in and vacationing in the Hamptons,” he told me. “She had minimal symptoms except she forgot to turn the chicken off and it almost burned the house down, and so her kids kind of tease her about her memory.” She had animals on the property; she had indeterminate test results. She had sore wrists and ankles that came and went. Her hands would feel numb in the morning. She had Raynaud’s — “That’s common in Lyme.” (According to the American College of Rheumatology, 10 percent of the population experiences Raynaud’s, a circulatory response to cold and stress.) In the past, she’d tried to get an Adderall prescription to help her focus.
“That’s a Lyme case until proven otherwise,” Raxlen said. “That’s certainly enough for me to put her on an oral-antibiotic program — come back, see me in two months.”
Raxlen is currently on a three-year probation with the New York State Board for Professional Medical Conduct over allegations that include gross negligence, gross incompetence, and failure to maintain adequate medical records. This is not the first time he has come to the attention of state medical boards; once, he was accused of telling a woman dying of Lou Gehrig’s disease that she might have Lyme. (He was ultimately not officially censored.) But his current probation does not seem to have injured his standing in the world of Lyme. This fall, he will receive the Pioneer in Lyme Award at the 2019 ILADS conference in Boston.
Connecticut in early summer is superabundantly green. This is the corner of the country where Lyme disease was first named: in towns that feel like the country without being too far from the city’s money, places with old stone walls and graveyards with ancient headstones like rows of buckteeth. In June, I took Metro-North to western Connecticut to visit a Lyme support group. The houses I passed on the way from the train station ranged from the ersatz niceness of Colonial McMansions to the historic niceness of Colonial landmarks.
The group met in a town building between the planning-and-zoning offices and a community playhouse, and its exterior — Georgian-style redbrick — conformed to the surrounding niceness. Its interior was universal municipal bleak. Tonight’s meeting would be a little unusual, the group leader told me when I’d asked if I could visit. It would be led by a Reiki master who specialized in Lyme and other tick-borne diseases. Seven women had come, all in late middle age, all with glasses and sensible hair.
To start with, the Reiki master suggested, perhaps we could go around and share our stories, say where we were in treatment — only if we were comfortable. She would go first. “I had Lyme and babesia back in 2005, 2006,” she said, referring to a parasitic infection frequently diagnosed alongside Lyme. “My son had Lyme, babesia, and bartonella — so we had multiple diseases, both of us.” In recent years, the doctors who treat chronic Lyme have placed an increasing emphasis on tick-borne “co-infections”; patients are urged to get tested for a broad range of other conditions, some vanishingly rare. Bartonella, for example, has not yet been shown to be transmissible from ticks to humans, but it is one of several co-infections widely discussed. (Mold poisoning also comes up frequently.) The Reiki master went on: “I was treated for 15 months on antibiotics; he was on them for eight months. Many, many, many different ones over the time period. And then we did some herbs and homeopathics. But the whole time, I was already a Reiki master, so I was always doing energy work.” Now, she said, “I’m symptom free, my son’s symptom free.” She rolled her chair so she could knock on the wood of a bookcase behind her.
A newcomer to the group said she was attending on behalf of her children. She had, she said, “an awkward situation.” Her eldest had suffered from serious psychiatric issues for years — she’d been hospitalized and had considered antipsychotics. And then last fall her younger daughter had come to her parents and said she hadn’t been feeling well. She was exhausted, forgetful, having panic attacks. She was afraid of turning into her sister.
She’d been to ten, 12, 15 doctors, and one of them seemed to think she had Lyme. Her parents took her to a naturopath who ordered an IGeneX test that came back positive and started her on herbs and a special diet. But the naturopath said she should probably be on antibiotics, too, so they took her to an LLMD. The LLMD said she probably had a co-infection. So, then, “more IGeneX — and they found out that she had babesia.” This daughter had seemed to be doing better now, though. The current problem was her eldest. After discussing her symptoms with an LLMD and reviewing files from her mental-health hospitalizations, they’d come to a conclusion: The eldest daughter had “full-blown psychiatric Lyme.” The problem was she didn’t want to be treated for Lyme disease.
This story took a while to unfold and the Reiki master wanted to make sure we had time for Reiki, so we didn’t make it the rest of the way around the table. But first, she recommended a New York neurologist who treated Lyme.
It was a name the newcomer recognized. “But you know what? She’s $1,200 an hour,” she said.
“Is she that much?” the Reiki master asked. “I think it’s just the first visit.”
A chorus: “She sees you initially, and then after that she puts you in with one of her associates at $600 an hour.” “The cost is a huge piece of this.” “It’s brutal.” “They’re all very expensive for the first appointments.” “They’re great doctors, brilliant people. When you sit with them for two, three, four hours, the depth they go into is profound.”
“There’s not enough of these Lyme-literate doctors,” the Reiki master lamented. Fortunately, she explained, energy healing provided techniques to try on your own, no doctor’s appointment required.
The group was interested. They were taking notes. If any of them wanted to come in for a session, she told them, she could give them 50 percent off her usual rate of $250. “I know everybody’s so hurting for money when you’re being treated,” she said. Between doctors and supplements and antibiotics — “and if you’re on Mepron for babesia, forget about it. It’s like ridiculously expensive.”
“We used to call it liquid gold!” said one woman. “My husband would yell at me if I spilled a drop of it.”
They were lucky, the Reiki master reflected, that Reiki had begun to find wider acceptance. A while back, there’d been a study at Yale showing that patients having heart attacks who received Reiki recovered more quickly than those who didn’t. “It was a great controlled study,” she said.
Her description captured a central tension of chronic Lyme: a rejection of mainstream scientific authority coupled with a desire for mainstream scientific legitimacy. As for the cardiology study, the Reiki master is not wrong. The medical establishment has not yet subscribed to a worldview that includes auras, but it is open to the possibility that this experience — someone touching you gently, focusing intently on your well-being — might be enough to measurably change the way your body functions, even if no one can quite explain why. But Reiki, in contrast to the practices of Lyme-literate doctors, presents no risk of actively harming a patient.
The support group, meanwhile, pulled in other directions. “I have a question,” one woman responded. “Can you spell that anti-malaria drug?”
“Mepron. M-E-P-R-O-N.”
“Does it make you sicker?”
“All of them can cause herxes,” the Reiki master said. “They all can, anything you take.”
Herxes, or “herxing,” are a great bugbear in the world of chronic Lyme.
The term is drawn from the Jarisch-Herxheimer reaction, originally identified in the context of syphilis. It refers to a brief, severe reaction that can take place within the first few days of antibiotic treatment; as bacteria die off and release endotoxins, a patient experiences fever, chills, and sometimes dangerously low blood pressure. A Herxheimer reaction is possible during treatment for Lyme disease, but in common use among chronic-Lyme patients, herxing has come to encompass any negative response to medication. Herxes could last for days or weeks and could recur cyclically during ongoing treatment.
The logic of the herx is familiar from the wellness realm of extreme cleanses and colonics: “Detoxing” is good for you, and it’s supposed to feel bad. More insidiously, though, within the context of chronic Lyme, the herx contributes to a sense of inevitability. If you feel better after treatment, that means it’s working; clearly you have Lyme. If you feel worse after treatment, that also means it’s working; clearly you have Lyme. No circumstance could ever disprove a chronic-Lyme diagnosis —any test is suspect, any treatment provisional, any cure potentially temporary. The all-encompassing certainty of Lyme was what unnerved me, but this seemed to be exactly what patients wanted. Lyme was certainty. Lyme was authority and answers.
I had been in the conference room for almost two hours, and the circularity of chronic Lyme had begun to make me claustrophobic. The women around me weren’t crazy or foolish. They’d done what anyone would do when something about your body doesn’t feel quite right: They’d gone to the doctor. They’d gone to a specialist.
But this doctor specialized in finding a particular disease, and, once found, the disease could explain everything. It engulfed any alternative. I knew that mental-health diagnoses were a difficult subject among chronic-Lyme patients; non-Lyme doctors who suggested a psychiatric basis for symptoms were a source of profound frustration. Such suggestions were understood to translate directly as All in your head, so get over it. There seemed to exist no acknowledgment that a patient in the grip of a major depressive episode might be unable to think straight, unable to move, unable to get out of bed — nor that telling such a patient to just snap out of it would be as useless as telling a flu patient to try having less of a fever.
Provided that the depression and anxiety were caused by bacteria, the support-group attendees readily described them as central facets of Lyme.
(“Psychiatric Lyme” is a term with little purchase beyond the Lyme-literate community. It relies heavily on the research of the Columbia psychiatrist Brian Fallon, who runs the university’s Tick-Borne Disease Research Center and otherwise specializes in “illness anxiety, hypochondriasis, obsessive-compulsive disorder, and somatoform disorders.” In addition to researching long-term antibiotics for Lyme, he has also done research on antibiotics as a treatment for psychosis.) In a large green box, a pamphlet reads, “It is important to remember that Emotional and/or Cognitive disorders can be the only symptoms of Lyme disease.” A list of possible manifestations includes depression, anxiety, irritability, rage, hyperactivity, and problems with attention and focus.
Aronowitz sees “a kind of irony” in the frustration that chronic-Lyme patients can inspire among mainstream doctors. “We set a standard that says something like, for your suffering to be legitimate and for us to pay attention to you and want to see you — this is ‘we, medicine’ — you should have a mechanism behind it. So are we surprised that there’s a whole lay group organized around saying we need a mechanism and we demand you see that there’s a somatic mechanism behind this thing?” He went on: “There’s suffering that has no name and no precise mechanism, possibly because it’s not localizable to a mechanism. And that doesn’t make it illegitimate, either.”

Blogger Jordan Younger on Instagram. Photo: Instagram
I arrived home from the meeting with a lime-green nylon bag printed with a large silhouette of a tick and the legend LITTLE TICK, BIG PROBLEM. I’d stuffed a handful of pamphlets inside and began to read them.
The pamphlets were produced with support from IGeneX and, in the case of the Lyme Disease Association’s LymeR Primer, a roll call of other tick-borne businesses: companies selling insect-protective clothing and tick-control systems and other diagnostic labs — among them Galaxy Diagnostics, the self-declared “Best in Bartonella Testing.” If Lyme can be an identity, it is also a market, not just for tick boxes and diagnostics but also for brands. On her website, the $1,200-an-hour neurologist recommended in the meeting sells $220 nutritional cleansing supplements and her own line of anti-tick clothes.
Jordan Younger is a wellness blogger who received a diagnosis of Lyme disease last summer, and since then she has been sharing updates about her condition and treatment with her 211,000 Instagram followers. Several years back, Younger began writing under the name “the Blonde Vegan,” but in 2014 she concluded that her veganism was a form of orthorexia — disordered eating — and rebranded herself as “the Balanced Blonde.” The episode of the Balanced Blonde podcast in which Younger discusses her Lyme diagnosis presents a survey of her lifelong health issues. Focused primarily on digestion and skin, the story begins in her infancy and leads inexorably to the offices of Dr. Erica Lehman, a Beverly Hills ophthalmologist practicing as an LLMD. (Her biography lists fellowships in corneal surgery.) Lehman tells Younger that she has “every right” to feel bad (“which was so validating and exciting,” Younger says). It all makes sense to her in retrospect: her lifelong food issues, her orthorexia. “I was dealing with these Lyme bugs,” she says, “taking over my body and eating all my nutrients.”
I spoke to Younger a little over a year after she was first diagnosed, and she described the treatments she had undergone since then. Right away, she said, Lehman started her on around 30 supplements and began doing ozone therapy, a procedure in which blood is drawn, mixed with ozone, and then reinjected into the body. Younger did ozone for nine months or so, and it always made her feel worse. “At first I was so okay with the Herxheimer reactions,” she said. “It’s part of healing. But I reached a point more recently where I really do just want to feel better in my everyday life.” So she stopped doing ozone and stopped some of the other drugs she was on, and lately she was getting injections of umbilical stem cells, plus thrice-weekly Rocephin IVs. She also goes on weeks-long “water fasts” at healing centers. Her doctor doesn’t send her on those; she does them on her own, but she has met fellow Lyme patients that way. When you fast, “it starves the toxins,” she explained.
Younger told me that Lyme has become her greatest gift. It opened her up to the things that really matter and gave her permission to draw boundaries and say no to things she doesn’t want to do. “I mean, I’ve said things to my family like, ‘Well, part of why I’m sick is because of the pressure that you’ve put on me my whole life.’ And my mom’s like, ‘Well, aren’t you sick because of a tick bite?’ And yes, that’s all true.”
Lyme has also brought the Balanced Blonde to a new audience. Instagram is home to an active Lyme community, and many of Younger’s photos are now hashtagged #lymewarrior; they receive hundreds of comments and thousands of likes. Target is among Younger’s sponsors, suggesting that perhaps Lyme content isn’t a bad way to reach wellness-minded American women. “Jordan younger lyme disease” is among Google’s top suggested searches for her name, along with “jordan younger age” and “jordan younger net worth.”
In late June, a draft of the new Infectious Diseases Society of America guidelines was released for a period of public comment that will run through August 10. They make a clear point to acknowledge the potential for persistent symptoms after treatment. The pain is real, and it merits attention; it’s just that no studies have yet shown that long-term antibiotics are the best way to heal it. To my eye, at least, the guidelines take seriously the experiences of Lyme-disease patients who have had complicated recoveries.
Abby Hartman, a pet trainer who lives outside Minneapolis, tested positive for Lyme disease after tick bites; her doctor gave her first one course of antibiotics and then another. But even after that, Hartman still had bad joint pain and frightening neurologic symptoms, like slurring her speech and forgetting her husband’s name. She was seeing mainstream doctors for her treatment — a rheumatologist, an infectious-disease specialist, doctors in the ER — but, of course, she was also Googling, and when she Googled she quickly found herself in the world of chronic Lyme. The things she started to read there were terrifying: They told her she’d be sick forever, that Lyme bacteria would stop her heart, that they’d drill into her eyes and leave her blind.
She joined some Facebook groups and got a recommendation for a Lyme-literate doctor over DM — members were careful not to post doctors’ names publicly out of fear they’d be targeted by state medical boards or insurance companies or the CDC. That doctor started her on muscle relaxants and a shifting combination of antibiotics that she’d stay on for the better part of a decade as symptoms came and went. At one point, she had diarrhea for three years straight, which her LLMD blamed on Lyme in her GI tract.
Not until her child got involved did she really start to feel uncomfortable about what was going on. An LLMD told Hartman that her young son probably had Lyme too. (The chronic-Lyme community entertains the possibility that Lyme could be transmitted in utero, and perhaps also sexually, neither of which mainstream research currently supports.)
Her husband was dubious, and when Hartman echoed his skepticism on Facebook, the backlash was swift and intense. People she’d thought of as friends accused her of medical child abuse; they threatened to call CPS. Plus, she’d noticed others talking about how people with Lyme shouldn’t get vaccines, which alarmed her — she believed in vaccines.
“So I started arguing about vaccines,” she told me. She started looking for more ways to push back. When someone would talk about how their daughter had lost a gallbladder to Lyme, Hartman would post a news story about a patient who’d lost a gallbladder to chronic-Lyme treatment. “It would blow everyone up,” she said. Earlier this year, she decided to write a blog post with the title “Lyme Warrior No More,” explaining why she no longer subscribed to the community’s beliefs. Afterward, people she’d been talking to for years accused her of being “a paid CDC shill.” (This conspiratorial register is not uncommon and is perhaps gaining traction. Earlier this month, a New Jersey congressman demanded an investigation into whether the government had developed Lyme-infected ticks as part of a secret biological-weapons program.)
Back when she was in all those Facebook groups, she said, “it made me feel like I was in the Matrix, and I took a red pill and I could see the truth.” It was hard to leave that sense of clarity behind.
Allie Cashel, the patient who wrote a book with Raxlen, has translated her experiences with chronic Lyme into political engagement. She now lives in Vermont, where she’s a fellow of the New Leaders Council, a group dedicated to training progressive millennial leaders. She lived in New York for a while but says her condition made the pace hard to take — her family has a house in Vermont, and when she was growing up, they’d drive there on weekends to ski. In Suffering the Silence, Cashel remembers watching as her father “self-administered IV antibiotics en route, one hand on the wheel.”
When Cashel and I spoke, I told her I’d read her book and was interested in the moments growing up when she seemed to feel skeptical about what was happening. There’s a period (in between stints of being treated by Raxlen) when she is receiving Rocephin IVs in a local doctor’s windowless basement. Her mom comes along with her for appointments and, at one point, the mom is feeling tired and achy, so the doctor starts giving her Rocephin too.
Even as a teen, Cashel senses something amiss. “If my doctor would treat someone who wasn’t sick,” she writes, “maybe I wasn’t sick either.” It seemed like Lyme-literate medicine could be sort of a Wild West, I told her. What did she make of all the risky treatments on offer? She worried about it, she said. In general, though, she advised people to pay attention to their instincts if something didn’t seem right. “You know if you’re in a space that is not super-safe,” she said.
This is not bad advice, as far as it goes, but it is also a little sad. It means, essentially, that the ethics of commerce apply even when you’re sitting in the examining room: Let the buyer beware. Yet it doesn’t seem unreasonable that patients should trust that their doctors are working in service of principles higher than securing a repeat customer. Polly Murray writes in The Widening Circle that she’d always revered the power of medicine; to come up against its limits was devastating. Acknowledging these limits is difficult — for doctors, for patients, for everybody. We’ve invested near-spiritual fervor in the medical realm: It holds our births and our deaths; it sees inside us and tell us what’s wrong.
After Hartman left Lyme, she started looking for an aggressively conventional doctor, and eventually one satisfied her standards. The new doctor talked Hartman through the side effects of all the drugs she’d been on and discussed ways they might handle her symptoms.
“She rubbed me the wrong way during our first conversation,” Hartman said of her new doctor, “because after we had talked about all this, she looked at me and said, ‘When would you like to come back?’ And I was really upset because I was thinking, Well, you tell me. What’s the plan? I mean, are you just not going to do anything?” It took Hartman a moment to make sense of the exchange. “She wanted to know, like, do I feel like I need to come back?”
“Whenever I went to the Lyme-literate doctors, I didn’t have to say a thing,” Hartman said. “I would come in and they would literally hand me a binder, and they were like, ‘This is your instructions.’ And under each tab, ‘This is the first week, this is your detailed plan, there is a handout about your exact condition, you’re going to come back every week at $300 each time you come.’ ”
That was what Hartman had liked. “It was just that being told what to do felt so good after people saying, ‘I don’t know. I don’t know what to do with you.’ ”
Sitting with her new doctor, Hartman had a realization. “I was waiting to be sold something,” she said. “I’m realizing this is exactly who I need to be with: someone who is going to make me think about it instead of just telling me what to do.”
- COVID UPDATE: What is the truth? - 2022-11-08
- Pathologist Speaks Out About COVID Jab Effects - 2022-07-04
- A Massive Spike in Disability is Most Likely Due to a Wave of Vaccine Injuries - 2022-06-30

